 I work in a teaching hospital. That means there are often residents and medical students involved in the care of patients. So when I have a consult, not only do I have to give my assessment and plan, I try and justify that assessment and plan with the literature.
I work in a teaching hospital. That means there are often residents and medical students involved in the care of patients. So when I have a consult, not only do I have to give my assessment and plan, I try and justify that assessment and plan with the literature.
But the literature is often less than clear cut.
There are those consults where my conclusion has the force and authority of the 10 commandments. Perhaps a bad metaphor. Some consults, like the treatment of MSSA endocarditis, result in an assessment and plan that is big ‘T’ Truth.
Others? Like how to treat MRSA endocarditis? Lots of depends (no incontinence jokes please) and requires an interpretation of a less than straightforward literature. These are times that I have to offer my best synthesis of the data. But my opinion is likely better than most.
Sometimes I have little to guide me. I have a weird bug in a weird place and no literature to guide me outside of a few case reports. All I have is the bacterial antibiotic sensitivity pattern and hope.
And sometimes I got nothing. I get asked a question that has no real answer, such as is the fever from infection? I don’t really know and I let the house staff know that my opinion is just that, an opinion informed by experience and bias, not evidence. And oddly, others often defer to my advice. Kind of scary. One of the few advantages of being old and grey, it gives the illusion of wisdom. I often say being a sub-specialist is being ignorant with style and authoritah.
But I need to be explicit when my opinion is just my opinion.
Sometimes papers are opinion wrapped in data, which is nice, as that is just what this blog is, but the medical literature, I think, tends to be read with the assumption that the journal articles are written are without bias, the opposite of a blog. Not always.
They reviewed the studies to date on the benefits of health care worker influenza vaccination and conclude:
The four cRCTs underpinning policies of enforced HCW influenza vaccination attribute implausibly large reductions in patient risk to HCW vaccination, casting serious doubts on their validity. The impression that unvaccinated HCWs place their patients at great influenza peril is exaggerated. Instead, the HCW-attributable risk and vaccine-preventable fraction both remain unknown and the NNV to achieve patient benefit still requires better understanding. Although current scientific data are inadequate to support the ethical implementation of enforced HCW influenza vaccination, they do not refute approaches to support voluntary vaccination or other more broadly protective practices, such as staying home or masking when acutely ill.
The studies, all done in long term care facilities (aka nursing homes) are admittedly relatively weak tea when taken in isolation from the rest of the vaccination literature. But it is the data we have.
They did not include “Influenza vaccination of healthcare workers in acute-care hospitals: a case-control study of its effect on hospital-acquired influenza among patients” from 2012, probably as it wasn’t an RCT. The only study in hospitals, it demonstrated benefit from HCW flu vaccination:
The median proportion of vaccinated HCW in these units was 11.5% for cases vs. 36.1% for the controls (P = 0.11); 2 (20%) cases and 21 (48%) controls were vaccinated against influenza in the current season (P = 0.16). The proportion of ≥ 35% vaccinated HCW in short-stay units appeared to protect against HAI among patients (odds ratio = 0.07; 95% confidence interval 0.005-0.98), independently of patient age, influenza season and potential influenza source in the units.
CONCLUSIONS: Our observational study indicates a shielding effect of more than 35% of vaccinated HCW on HAI among patients in acute-care units.
The authors of the review do declare their bias behind the review up front:
The ethical premise for mandatory HCW influenza vaccination critically hinges upon the valid demonstration of patient benefit substantial enough to justify infringement of the personal rights of HCWs who would otherwise choose not to receive influenza vaccine each year.
What, I wonder is substantial enough?
So I start with an entirely different premise/bias for my take on the literature. I approach the problem from a patient safety perspective and start with the issue of patient harm. What is the result of hospital acquired influenza?
Answer?
Death.
influenza A (H1N1)pdm09 infection (odds ratio: 1.63; 95% confidence interval: 1.37-1.99)…CONCLUSION: Influenza A (H1N1)pdm09 infection acquired in the hospital is an independent factor for death in critically ill patients admitted to the ICU.
And:
in children with severe viral respiratory infection, hospital acquisition of infection is associated with increased mortality even after adjusting for chronic medical conditions that predispose to an increased risk of complications from viral illness.
And:
Influenza virus pneumonia (3 patients) and attributable mortality (2 patients) during active infection was observed in patients with lymphocytopenia at onset.
Although others have demonstrated less mortality in retrospective studies but all have the patient morbidity of a week or two of influenza.
But killing patients by giving them influenza is, to my mind, a bad thing. What is an insubstantial number of deaths from flu acquired from HCW’s such that no vaccination is required? For me? Zero.
Hospital acquired influenza does happen, although rarely:
The overall incidence of hospital-acquired respiratory viral infection was 3.9 (95% confidence interval, 3.7-4.1) cases per 1,000 admitted patients. Rhinovirus was the most common virus (30.3%), followed by influenza virus (17.6%) and parainfluenza virus (15.6%).
Of course, knowing the influenza is acquired in the hospital is one thing, knowing if the patient acquired influenza from a health care worker is quite another. Often, we do not know just where the patient acquires her influenza:
Unobservable transmission was the main cause of HA-ILI transmission suggesting that symptom-based control measures alone might not prevent hospital outbreaks.
And more exposure is worse the less:
Hospitalization in double-occupancy rooms and the risk of hospital-acquired influenza were assessed prospectively. The incidence was 2.0 for 100 patient-days in double- vs. 0.7 in single-occupancy rooms (p 0.028).
So hospital acquired influenza is rare, difficult to determine the source, can be fatal, results in morbidity and is hard to control.
And I will note there is often an odd disconnect between morbidity and mortality from hospital acquired infections and taking responsibility for that morbidity and mortality. I suspect is part of why infection control and prevention guidelines are sometimes forgotten or ignored. There is an institutional responsibility (in my institutions we ‘deep dive’ into every infection) but not a personal responsibility, as would occur if a patient had a fatal overdose or a doctor put a chest tube trochar through the heart. If we could only know who passed on the organism that caused infection and when it occurred, guilt would be so much simpler. So who gave the patient the influenza that killed her? We never know and it takes the edge off of the responsibility for some.
In my own experience, and I am not immune to the dangers of anecdotes, in my 27 years we have had one influenza outbreak that we could credit to a HCW, unvaccinated, who came down with symptoms in the middle of his 12 hour shift. No one died although there was significant morbidity. And to the best of my memory we have never had a death from nosocomial influenza in my hospitals.
And:
Nearly half of HCWs with influenza were afebrile prior to their diagnosis. HCWs with respiratory symptoms but no fever may pose a risk of influenza transmission to patients and coworkers.
Making waiting for symptoms to intervene problematic.
As a health care provider the dominant ethical imperative is to protect my patients. It is the first law: A robot, er, I mean, health care worker may not injure a human being or, through inaction, allow a human being to come to harm.
I wonder. Is there a relatively effective way to prevent the spread of influenza? I would suggest the flu vaccine. I have written buckets on the flu vaccine on this blog, so my summary. All the data points the same direction: the flu vaccine decreases the chance of acquiring the flu and if a HCW does not get the flu they are not going to pass it to their patients. And kill them. Plus, a vaccinated HCW is potentially one less vector in the community, adding to herd immunity, such as it is with flu.
Is the bang worth the buck? That is a question I cannot answer. What is one life worth? We do a lot of things in the hospital to prevent complications that have a low probability from occurring but have a high morbidity and mortality. And if I have learned one thing in 30 plus years of infection control, there is no one intervention that will prevent infections, it is the summation of many interventions.
I do think our primary moral imperative is to not kill our patients with vaccine-preventable illnesses and that is the more important ethical imperative, not HCW autonomy.
But that is me.
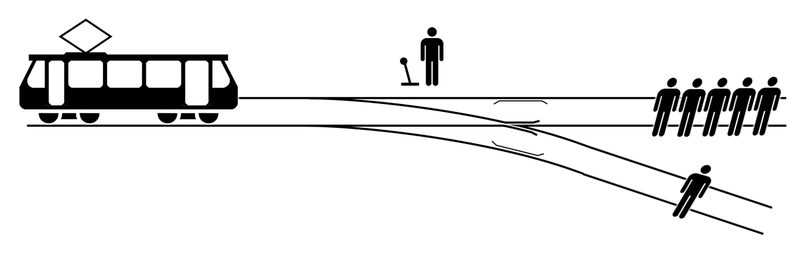
It would be interesting to come up with a series of vignettes, like the Trolley Problem, to see where most people stand with the ethics of HCW vaccination. In the meantime I’ll let you hash it out in the comments.
Prior flu ramblings
- Scam Stud
- The Tamiflu Spin
- Yes, But. The Annotated Atlantic.
- Cochrane Reviews: The Food Babe of Medicine?
- One Flu Into the Cuckoo’s Nest*
- Uneasy Lies the Head That Wears the Flu
- What are words for?
- I refute it thus
- Protect Yourself
- Drinking from the Fire Hose: Odds and Ends on the Gasping Oppression
- Random Flu Thoughts
- Ososillyococcinum and other Flu bits.
- Influenza Vaccine Mandates
- Nine Questions, Nine Answers
- Flu Vaccine Efficacy
- More Flu Woo for You Boo Boo.
- Herd Immunity
- Flu Woo Hodge Podge
